Analysis and Rationale in Patient Selection for Laser Vision Correction
by David A. Wallace, M.D.
Laser vision correction surgery can be a significant life-changing event. On the positive side, it can help someone who previously was dependent upon eyeglasses and/or contact lenses to achieve excellent unaided vision. This is why in less than 6 years LASIK has become the most popular elective surgical procedure in the world.
We have all seen the “infomercial fairytale” promoting LASIK, which goes something like this: Someone chooses to have LASIK; seeks a consultation from caring and capable provider; has a few minutes of painless surgery; achieves overnight recovery of extremely clear vision; and lives happily ever after.
What we do not hear much about are the stories of those that have problems and complications as a result of laser vision care. Some patients achieve clear vision (“20/20” on the eye chart) but observe annoying glare, halo, and difficulty with night vision after LASIK. Some patients fail to achieve optimum vision in both eyes and find that their depth perception, driving comfort and other factors are impaired. If surgery is performed in certain situations where corneal anatomy and shape are abnormal, or if significant surgical complications are encountered, it can lead to severe vision impairment, need for rehabilitative surgery including corneal transplantation, severe psychological stress, depression, loss of work, and diminution of quality of life. Neither positive or negative effects of this care should be underestimated.
This section was written to review what is known about evaluation of candidacy for laser vision care, and when it may be inadvisable or contraindicated to be supportive of such care for particular candidates. Specifically, we will review here cases of high astigmatism and unusual corneal shape as measured by topography and aberrometry devices.
Keratoconus is a corneal condition characterized by abnormal shape, abnormal curvature steepening, and focal corneal thinning. This can be seen when imaging the cornea with topography or dual-surface imaging systems. An asymmetric topography pattern is the hallmark of keratoconus and related entities like Pellucid Marginal Degeneration. The abnormal corneal shape causes direct optical consequences — instead of the cornea acting like an optimal lens in the eye’s visual system, it acts somewhat like looking through hand-blown glass, with consequent distortion, irregularity, and other imperfections that can’t be corrected by eyeglass lenses or soft contact lenses. Keratoconus can often be progressive, therefore placing the afflicted individual at risk for progressive visual deterioration. Fortunately, a new treatment is available that can strengthen affected corneal tissue, referred to as UV Corneal Collagen Cross-Linking or CXL for short. We offer CXL care at LA Sight as a part of an ongoing investigational study, the CXL-USA Study Group.
This content reflects the clinical judgment and medical opinions of the author, and is not intended to represent an exhaustive review or authoritative literature survey. It is presented here primarily for teaching and informational purposes.
Before reviewing the following material, one should have a reasonably sophisticated working knowledge of eye anatomy, refractive optics, and corneal topography.
Case 1
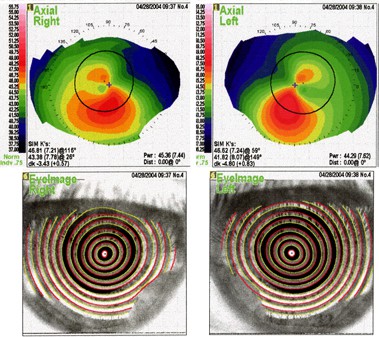
23yo male seen 04/04
OD: -4.00 -8.00 x 168 (20/40)
OS: -0.25 -6.50 x 180 (20/25)
Pupils 6.0 OU
Pachymetry OD: .475 (ultrasound), .431 (Orbscan); OS: .511 (ultrasound), .461 (Orbscan)
Topography reflects reasonably symmetric astigmatic hemi-meridians , so on the basis of the color printout alone one might think this would not disqualify from candidacy. However, look at the Sim-K readings just below the topography image. K readings OD are 45.73 x 53.40 @ 78, and for OS are 42.29 x 49.20 @ 90. These K readings alone should raise a significant “caution flag” in the mind of the refractive surgeon, as keratoconus by some definitions includes any cornea with a maximum K of 50D or more.
Orbscan studies in corneas like this are certainly appropriate, if not “standard of care”. These studies are shown below.
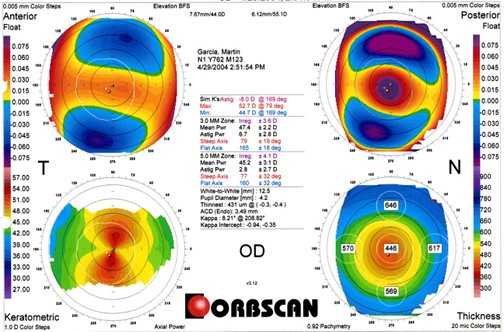
In addition to the very high astigmatism on Keratometric map (lower left map), the posterior float (upper right) shows very significant posterior bulge exactly in the areas where curvatures are highest (violet on the map). This is exactly the axis that would, if treated by laser, be sculpted to the greatest extent. Taken together, especially in the context of the corneas being thin to begin with, I felt this patient should not have laser refractive surgery.
Dx: Keratoconus
Recommendation: Not a candidate for laser refractive surgery.
Case 2
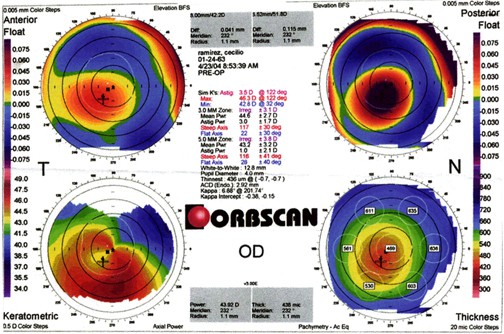
47yo female seen 03/04
OD: +0.50 -6.50 x 055 (20/40-)
OS: Plano –4.75 x 111 (20/25-)
Pupils 6.0mm OD, 6.5mm OS
Pach .412 OD, .433 OS
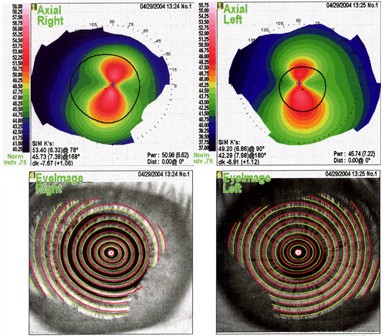
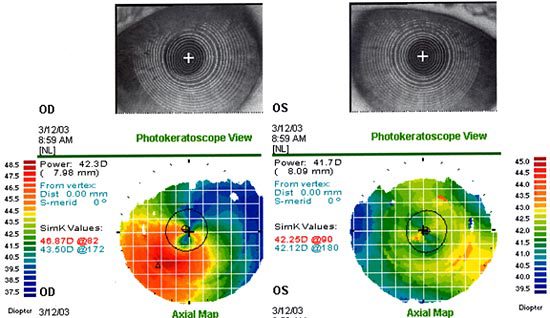
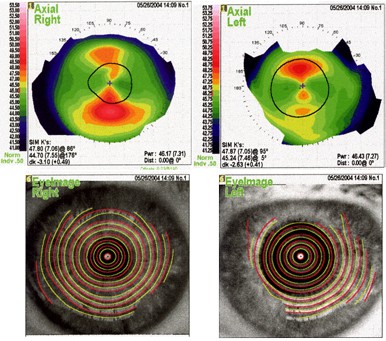
Topography is shown below:
Note the profound inferior steepening in association with profound central flattening in a near-vertical meridian. Also note the very distorted “tear-drop” appearance on photokeratoscope view.
Diagnosis: Pellucid Marginal Degeneration, both eyes
Recommendation: Laser refractive surgery would be contraindicated in this case.
Case 3
54yo male seen 03/03
OD: +0.75 -2.75 x 070 (20/20-)
OS: -0.25 -1.00 x 088 (20/20+)
Topography is shown below in both Axial and Elevation views.
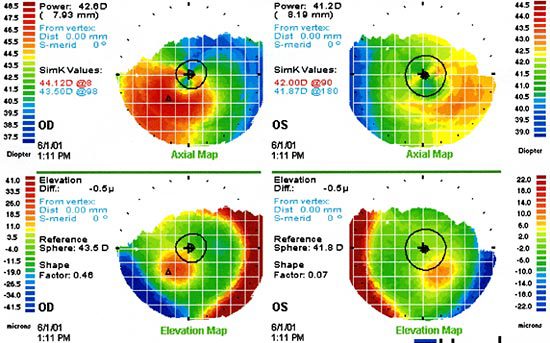
Note Asymmetry and eccentric area of elevation OD, not OS
Impression: Obvious corneal asymmetry OD, likely “form fruste (borderline) keratoconus .
Recommendation: Advised against laser refractive surgery.
Case 4
30yo male seen 11/01
OD: -2.25 -8.00 x 095 (20/60-)
OS: -2.75 -8.00 x 107 (20/60-)
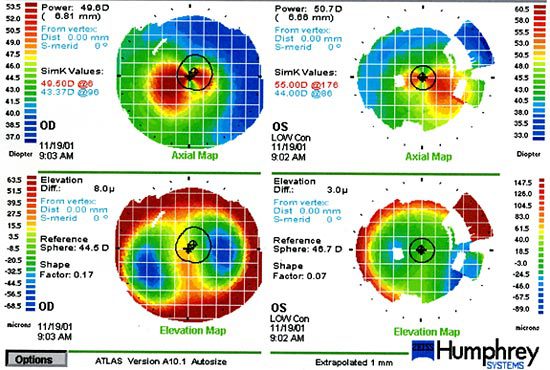
Diagnosis: Advanced Keratoconus, both eyes. Not a candidate for laser refractive surgery.
Recommendation: We fit this patient with rigid gas-permeable contact lenses and he now enjoys 20/30+ acuity OD and 20/25+ OS .
Case 5
27yo male seen 05/04
OD: -5.25 -4.25 x 176 => 20/20-
OS: -7.75 -4.50 x 178 => 20/20-
Pupils 6.75mm OU
Pach OD: .534, OS .557
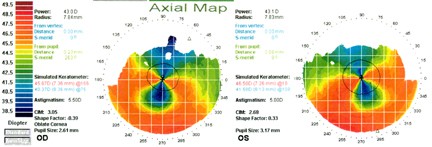
Topography is shown below: below:
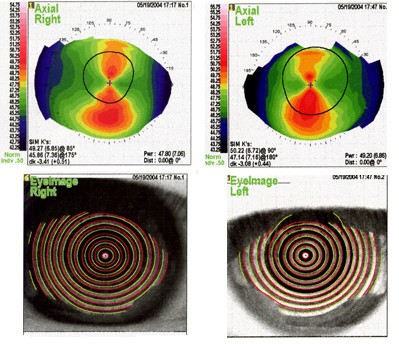
Diagnosis: Symmetric (though large magnitude) astigmatism, without evidence of keratoconus, pellucid, or other (asymmetric) shape disorder.
Recommendation: We are supportive of laser corrective care for this individual.
Case 6
38yo male seen originally in 05/01 and again 03/04
OD: -0.75 -3.25 x 033 (=> 20/30+)
OS: +1.25 -3.75 x 135 (=> 20/25)
Pachymetry (Central) OD .468, OS .535
Pachymetry (Inferior) OD .453, OS .483
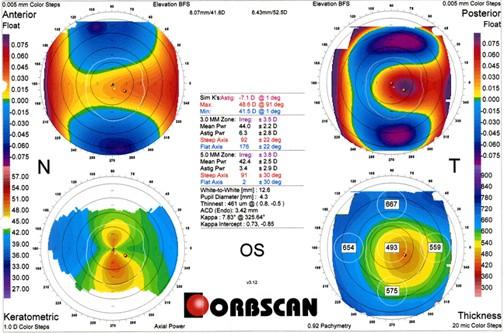
Topography:
Note the very asymmetric astigmatic hemi-meridians on axial map and the ovoid or egg-shaped ring reflection on photokeratoscope view.
On the basis of the thin corneas and topography map above, it might have been sufficient to disqualify this candidate from laser refractive care. We also obtained Orbscan studies, shown here:
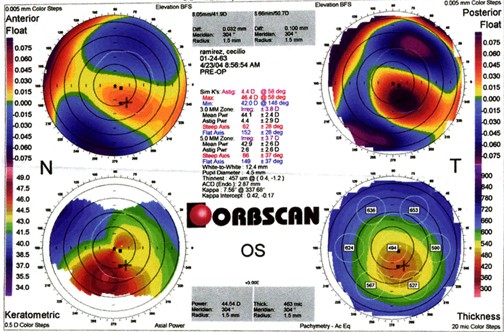
These studies are notable for eccentric thinning, with the thinnest portion of the cornea inferotemporally located in both eyes. There is also abnormal posterior surface bulge in both eyes exactly in the same location as the maximum thinning.
Impression: Keratoconus
Recommendation: Regrettably, we could not support laser refractive surgery in this individual.
Case 7
60 you female originally seen 06/98.
OD: +3.50 -7.50 x 009 (=> 20/20-)
OS: +3.50 -7.50 x 162 (=> 20/20-2)
Pupils: 5.0mm OU
Pachymetry: .535 OD, .529 OS
Topography is shown below:
This case is illustrative of an extraordinary amount of astigmatism. The good news is that it is perfectly symmetric astigmatism.
Diagnosis: Mixed hyperopic astigmatism
Recommendation: I first saw this patient in 1998. At that time, no lasers had FDA approval for treatment of mixed hyperopic astigmatism. The approval for this treatment occurred in about 2001, but because of the large magnitude of the treatment I deferred on treatment until mid-2003. After enhancement in 11/03, this patient is now a very happy uncorrected 20/25+ OD and 20/20- OS.
Case 8
56 yo female originally seen 01/02
OD: -5.00 -2.50 x 006 (=> 20/25+)
OS: -5.50 -0.50 x 160 (=>20/30+) at 01/02, changed to
OS: -5.75 -2.50 x 166 (=> 20/25-2) at 05/04
Pupils 5.5mm OU
Pachymetry .549 OD, .529 OS
Mild nuclear sclerosis OU contributing to 1-line loss of BCVA OU
Topography is shown below:
This case is interesting for two separate reasons:
1. Suggestion of significant refractive instability OS, with ~2.0D increase in astigmatism. In fact, this patient had been found to have an inferior retinal detachment at the time of her dilated fundus exam prior to the original evaluation, and was referred to a retinal specialist at that time. She needed scleral buckle surgery to repair the detachment, and the presence of the buckle is inducing the astigmatism! There is no better example I know of to justify performance of a complete dilated fundus exam at the time of laser vision correction consultation or surgery scheduling.
2. Suggestion of less than 20/20 BCVA should raise a caution flag (rule out keratoconus, etc.) except when another obvious explanation exists, such as mild cataract.
This patient had her detachment repaired in 02/02 and has scheduled her laser vision corrective care for later this year (’04). She has also been offered the option of cataract-style surgery but has indicated a preference in favor of LASIK at this time.
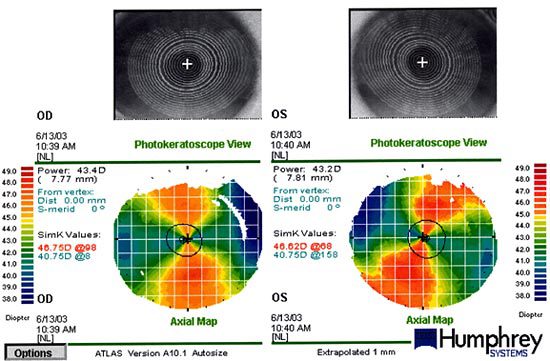
Case 9
33 yo male seen 01/01 by another surgeon.
OD: -3.75 -1.75 x 70 (=> 20/25-)
OS: -2.75 -3.25 x105 (=> 20/25-)
Pupils 5.5 mm OU
Pachymetry .508 OD, .505 OS centrally.
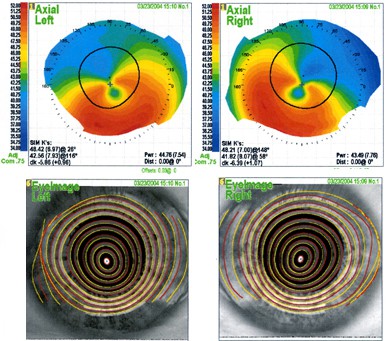
Topography is shown below:
This patient had topography clearly indicative of pellucid marginal degeneration as of the evaluation in 01/01. Unfortunately, the examining surgeon failed to appreciate this, and performed LASIK OU. Laser treatment was rendered to the right eye but a buttonhole flap was encountered in the left eye. The patient noticed poor vision beginning day 1 post-op OU, and progressive deterioration followed. He has subsequently needed corneal transplant surgery bilaterally and is still not completely visually rehabilitated. This case has resulted in litigation against the original surgeon.